I was diagnosed over a year ago with an Irritable Bowel Syndrom (also called functional colopathy, IBS, Irritable Colon Syndrom or ICS for those in the know). For about 6 months, I was continuously sick.
I will tell you the story of my chaotic (and sadly common) medical journey with this disease, which strikes about 10% of the world population (source). I’m also going to tell you about its important negative and positive impacts on my life.
Today, I’m much better. After meeting many doctors and specialists, I have finally found the personalized diet which allows me not to be sick anymore. It was mainly thanks to the help of a dieticien and by reading many articles. I also spent a lot of time finding the links between my episodes and my meals.
For a long time; I was reluctant to openly talk about my disease because I was afraid it could harm me one day. But after a post on Twitter, a lot of comments encouraged me to do so and convinced me it was useful. The lack of information and support by doctors seems unfortunately very common.
I wrote this article in order to:
- Encourage and maybe give some ideas to people with the same disease
- Show doctors that some existing diets works. It’s not inevitably about stress. It was useless to recommend alternative medicines to me.
- Show the medical field that, like many patients, I have wasted a lot of time because of the lack of information and doctor’s support.
- Add a witness for the press, patient associations and doctors and show them the urgency for doctors to get training, for the food industry and restaurants to adjust and ease the life of low-FODMAP diet patients, to show the importance of getting sure, true and updated information in French on the web.
- Help to talk openly about intestinal diseases.
- Thank my entourage who support me and adapt to my constraints.
Act 1: Symptoms Emergence
All seemed to begin on May 12th, 2018. It was about 7 p.m., I was having a cocktail dinner at home with some common foods: some French cheese (Comté, Ossau-Iraty), hummus, bread and beer. Around the end of the evening, I began to feel nauseous and to get abdominal pain.
The next day when I woke up, I felt more nauseous. I was not hungry at all. I forced myself to eat a little bit of white rice at lunch and, at the end of the afternoon, all got right back and I could normally eat again.
Everything was fine in my life. My job was going well and I was going on vacation in the next few days. Nothing was a source of stress for me.
May 15th: For lunch I was preparing a salad, again with some common products: lettuce, tomato, pepper, beetroot, seeds, cereal mix and dried vegetables. At the end of the afternoon, I got nausea and abdominal pain again that lasted all evening. The next morning, my health got back to normal.
But the same thing happened on may 18th and 24th… After each episode, I naively tried to change my diet based on what I read online. I tried to eat less acidic, less fat, to follow a diet advised by a gastroenterologist but nothing got better.
At the first episode, I guessed it could be due to a virus, a gastroenteritis, or food poisoning… But with time it looked like nothing I had ever known. As soon as I came back home from vacation, I decided to see my general practitioner (GP).
I took the habit of writing everything I ate, my symptoms, and my episodes. That allowed me to easily explain the situation to my GP and check any link with food. You’re going to understand its usefullness!
Description of my usual episode
All attacks looked alike. Intensity and duration could vary, but it usually started with nausea (that gradually appeared in about 1-2 hours), then tiredness. Nausea lasted for some hours. I rarely skipped more than one meal. Most of the time, I postponed my meal for few hours. It could be along with variable intense abdominal pain and bloating.
Then, usually, I got some intestinal disorders and abdominal pain for few days. Then everything got slowly better.
Unfortunately, I rarely got back to a normal state. Usually, a new episode appeared before the previous one completely disappeared.
Act 2: The first disapointment

At the end of May, I went to my GP. I showed her my diet diary, but all seemed right to her. She supposed it was a acidic stomach disorder and prescribed, for few weeks, a treatment with an impressive name: a proton pump inhibitor drug called Lansoprazole in French.
I don’t remember this period very well, but I think I didn’t get any episode until the beginning of July. I thought the drug was working at first but, unfortunately, the episodes reappeared at the beginning of July while I was taking this treatment for a month.
Episodes were linked and overlapped.
Act 3: Failed attempts of GP
It was summerime, either my GP or me went on vacation alternatively. So, I consulted different GPs.
Mid-July, I was on vacation in the Pyrenees. I decided to consult a local GP because I’ve been in pain for one week and the long treatment prescribed by my GP wasn’t working at all.
I explained the regular episodes I got since the last 2 months. This GP prescribed me a wormer treatment (Fluvermal in French) and charcoal against bloating.
No effect at all.
The impact on my life was quite important. I often felt pain and regularly tired. As attacks could happen in a matter of minutes/hours, I often cancelled my outings with my entourage.
I finally decided not to plan anything ahead. I dropped all my summer projects. I saw my entourage less and less. This disease started to isolate me.
I got more and more episodes and they were linking up. I rarely spent a day without symptoms.
Back from my vacation, I got a new episode. I consulted my GP and she prescribed a treatment against gastric reflux (SODIUM ALGINATE/SODIUM BICARBONATE) and a yeast (Saccharomyces boulardii) in order to go over my intestinal disorders and restore my intestinal flora.
No effect at all.
At the end of July, I consulted GP emergency because I was getting an attack during the weekend. It was more painful than usual and my GP was on vacation. For this GP, nothing was alarming and he prescribed me Spasfon and a blood test (which results were normal).
Spasfon had no effect.
Consulting different GP was exhausting. Each time I had to explain my situation again, show my diary, detail what the previous GPs ever did.
Many of them only focused on stress factor. I often had to argue that stress was not what made me sick. Some of them even argue that I could have been stressed unconsciously.
Regularly, they stepped out of their expertise fields by suggesting some alternative medicines: naturopathy, homeopathy, acupuncture… which I categorically refused.
At the beginning of August, after a few days of serenity, a new crisis came. I went again to see my GP who was back from her vacations at least.
She took things seriously and sent me for an echography. Results: normal.
I also went for a stool analysis. Results: normal.
Then, she sent me for a last test for Helicobacter Pylori Infection and said that she would send my to consult a gastroenterologist if the result was negative.
One week later, the resultats came back, negative.
I went back to my GP and she gave me a letter to consult a specialist. At that time, I was pretty confident, about a possible solution. I was impatient to meet the specialist in order to finally find why I was so sick.
I made my first phone call but they proposed an appointment several months later.
While my disease was ruining my life, preventing me from working and getting a social life, doctors all agreed that there was no emergency. I just had to take my pain patiently.
I spotted a practice that proposed an appointment at the end of September. This was by far the best date. I have a long month to wait…
I asked them if they sometimes had some cancellations. They answered me positively and advised me to call when I want to check if they had any cancellation. I called them twice a day… until I got an appointment on September 5th.
Act 4: The reserved diagnosis of the gastroenterologist
September 5th: I was happy to finally explain my situation to a specialist.
But I was quickly disillusioned. The consultation was cold and fast (15 minutes). The gastroenterologist didn’t know if the problem was due to the stomach or the intestine. So she decided to prescribe a treatment for both. I left her with very few additional information and a 3 months renewable prescription:
- Aflorex (one month): food supplement used to balance the intestinal microbiota
- Bedelix: digestive clay dressing
- Meteospasmyl: antispasmodic and a silicone dressing
- Imodium: antidiarrheal
- Trimebutine: regulates intestine motricity
At the end of the appointment, I asked her if she knew what I had. She told me it could be a stomach inflammation, functional colopathy… (the list went on)
The functional colopathy was one of the most probable hypothesis according to her. If so, she told me that the treatment should help me and that, anyway, she wouldn’t be able to do much better.
Some astonishing food recommendations
She also gave me dietary advices to regulate my transit and therefore reduce my pain and my episodes:
– 2 fresh kiwis on mornings, preferably on an empty belly
– Pineapple juice
– Non-whole grains at breakfast
– Mineral water (brand HEPAR) up to 1 liter a day
– Oil RESTRICAL to spice hot meals (do not cook)
– Spinach
– Oleaginous dry fruits (nuts, hazelnuts, almonds, …)
– Cooked prunes on the evening (3 to 4 with cooking juice)
– AXAROLA, one pill an evening
– FRUITS AND FIBERS, one pill an evening
This came from a very good intention, except that with a suspicion of functional colopathy, it was absurd (in my opinion) for several reasons.
I’m going to explain my point of view later below, but when you have a colopathy, it is often beneficial to remove (or at least diminish) FODMAPs from your diet. The efficiency looks obvious: a study showed that a low-FODMAP diet had a beneficial effect on 86% of patients.
FODMAPs are different types of molecules which are poorly digested by the small intestine and can therefore ferment in the large intestine. FODMAPs are generally divided into 6 categories: fructose, lactose, mannitol, sorbitol, galacto-oligosaccharise (GOS) and fructans. FODMAP tolerance varies depending on the person.
Now that you know that, let’s go back to the list. Many products are rich in FODMAPs:
- Cereals: wheat contains fructans, oat contains GOS
- Olaginous dry fruits: nuts contain fructans, hazelnuts, and almonds contain GOS`
- Prunes: they are rich in fructans and sorbitol
- AXAROLA: one of the main components is marshmallow which is rich in fructans, fructose, and lactose
- FRUITS AND FIBERS: one of the main components is fig powder, yet fig is rich in fructose.
I didn’t know at that time but discovered a few months later that functional colopathy made me become intolerant to fructans and GOS. So this diet was making me sick (she should have known it).
So you may have understood that this diet and treatment had no beneficial effect on me. On the contrary, I suffered one episode after the other and was in pain very often. I was still not able to plan anything. I was worried about my situation. I isolated myself. I hardly invited my entourage at home. Each time I planned to go out, I warned everyone I could cancel at any time. I was often not able to work because of the pain. I stopped all of my outdoor activities (like guitar lessons, sports, …).
A few days later, I got a big attack during the weekend. I was worried. My gastroenterologist didn’t have any free slots for a while. My GP had done everything she could.
Following a friend’s advice, I called 112 and talked to a doctor for about 15 minutes. We did an update on my case.
He explained to me that if I went to the emergency room, I could have an appointment with a gastroenterologist much faster and thus won a precious time….which was not true!Once there, after a few hours, I met an emergency doctor who kindly explained that I was not considered an emergency at all and I had nothing to do here. To treat the pain, he prescribed me TRAMADOL, a level 2 painkiller, which I decided not to take.
A new stupid diet
I rescheduled an appointment at the end of September with the gastroenterologist. She suggested me to do a gastro-colonoscopy in order to rule out any other disease (like Crohn’s disease) and try to put a diagnosis. Indeed, the diagnosis of colopathy is deduced by elimination. It is called a « functional » pathology because of the normality of the exams and especially of the colonoscopy, which do not find any abnormality explaining the symptoms.

She also gave me a document, written by a working club composed of hepato-gastroenterologists, which detailed a more precise diet than the previous one. There were 3 parts: dyspepsia (digestive disorder of stomach), functional colopathy or « irritable bowel », and bloats and digestive gas. As she wasn’t still able to put a precise diagnosis, she told me to follow all three.
This document was problematic to me for several reasons.
First of all, it was an exclusion list. That’s a personal opinion, but this kind of list is not practical at all when having to follow a strict diet. Then, it contained a section suggesting phytotherapy, an alternative medicine. At the same time, I was watching Richard Monvoisin’s Zététique & Intellectual Autodefense course (French). I quickly ignored this part.
Finally, this document was made in 2009. Since then, we had obviously made a lot of progress concerning FODMAPs. Sometimes the document advised to eat whole grains bread (which contains fructans and GOS), spelt (which contains fructans),…The exclusion list was not sufficient at all. It was easy to find food that were not forbidden by the list that contained FODMAPs. Finally, FODMAP were not even mentioned, so I couldn’t do any further research.
Having done previous research, I asked her what was the link between the document and FODMAPs. She replied that the list allowed us to avoid FODMAPs… which was wrong.
This second diet was not only inefficient, it also made me sicker. As the diet was very strict, I put my flexitarism aside. Sometimes, I bought some fish. I also regularly ate meat and fish in restaurants because, as vegetarian meals, I had only found cucumber makis and Breton spinach crepes.
Like the first time, the appointment was cold and fast. I left her with still many unanswered questions and I was afraid to do a gastrocolonoscopy in such conditions. I got a prescription for MOVIPREP (a solution for gastrique lavage) and PINAVERIUM, a new antispasmodic to try and stem my frequent and intense abdominal aches.
As with the previous ones, I didn’t feel any effect from the antispasmodic. It quickly joined my growing collection of medications that I had only used a few times before putting them in a box. The episodes continued to overlap and even intensified.
The gastro-colonoscopy
At the beginning of October arrived the time of the colonoscopy. At around 8 p.m. the day before, I had to drink 1 liter of Moviprep but was quickly disgusted by the taste after a few gulps. I didn’t have a good time, but I did it.
Neither the specialist nor the pharmacist had explained to me what to expect after that. How long until the effect strikes? How long does it last? I discovered it live!
Actually, the medication took 3 hours to begin to act (so around 11 p.m.), and lasted a good part of the night. After a very short night, I woke up at 7 a.m. to take my second take of Moviprep.
A friend of mine had to come in the morning to bring me to the clinic. Given the effect delay after the first take, I was very worried about the war trip that awaited. In the end, the trip was quite short and timing was not so bad.
In the operating room, I met my specialist who didn’t care to say hello and was indifferent. Without any previous indications, she just injected me with the general anaesthesia and the exam went fast. When I woke up, I was offered a meal….which contained FODMAPs (notably some white bread).
My gastroenterologist was supposed to come and see me just after. But time went by and I had no news. I would learn a bit later that she finally left the clinic without a warning. I tried to reach her by phone but she didn’t answer.
The effect of the anesthesia weared off, I had no pain due to the examination. I went home in the afternoon.
Her « diagnosis »
In mid-October, I had an appointment with her to check in. There was nothing significant. She told me there was nothing to do.
Her explanation was both short and vague and didn’t fit reality. I insisted to get some more explanations from her about what I suffered from. She cited 5 very distinct illnesses that I may have: dyspepsia, functional colopathy, Crohn’s disease (but that was unlikely)…. She mostly told me about my stomach and prescribed me BEDELIX and ESOMEPRAZOLE (a gastric antisecretory protons pump inhibitor, therefore meant for the stomach).
I felt like I did not make any progress. I was pissed. For more than 3 months and a half now, my belly hurt me all the time.
I was expecting much of these exams. I thought we would find what I had, yet I really felt the diagnosis was not right.
Act 5: A second gastroenterologist put a diagnosis…and that’s all!
As I anticipated the pseudo-diagnosis of my gastroenterologist, I also took an appointment with another specialist in order to have a second opinion.
This time, the specialist was more empathetic. He was rapidly sure that it was a functional colopathy. I therefore didn’t have a « serious » disease, in the sense that it didn’t have an impact on my life expectancy. He told me a little bit about that disease and wrote a letter to my GP.
As he put a real diagnosis, I asked him what we could do. He answered that « I had to be my own doctor » and there was nothing special to do. I confess that this sentence stayed on my mind for a long time!
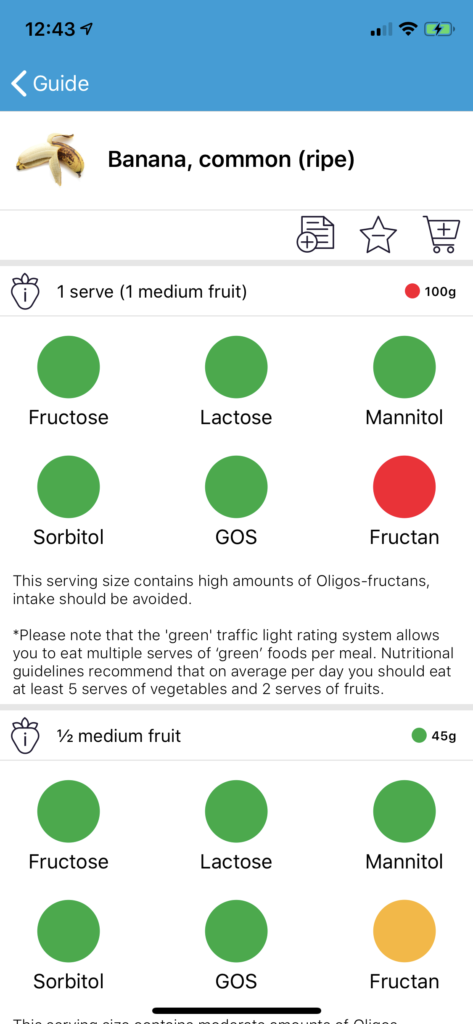
He gave me a document with some dietary advices (again an exclusion list). Then again, I would understand later that this list wasn’t updated (or was wrong) and far from prohibiting all FODMAPs. From my memory, this list advised to eat bananas, but ripe bananas are rich in fructans for example.
In the end, I was devastated by such lack of solution. I was regularly in pain, spending my time standing people up, I couldn’t plan anything… and there was nothing I could do about it.
At the end of the appointment, I insisted on trying other things. He wrote me on a post-it the name of a physiotherapist who was used to deal with that kind of patients. I took an appointment with this physiotherapist.
The gastroenterologists’ diagnoses seemed approximative to me, we were far from the National French GastreoEnterology Society (NFGES, SNFGE in French) recommendations. They never mentioned the Rome’s criteria or the Francis’ score. The emphasis was mainly on diagnosis, but not on support. They never proposed me any long-term follow-up. They never told me about APSSII (a French association for patients suffering from IBS) even though I asked if such thing existed. I had to ask for some medication to treat the symptoms.
Act 6: The physiotherapist who makes me waste my time
At the end of October, I got my first appointment with the physiotherapist recommended by the specialist. She was an expert in abdominal pathologies. She told me that she regularly accompanied colopaths and regularly saw improvement.
I showed my diet diary and nothing shocked her. After a few sessions, she deduced from my feedback that my problem was not linked to my diet.
She was empathetic. We talked well. She remained confident and that reassured me. I finally felt heard.
But she advised me to cancel the appointment I took with a dietician specialized in IBS and FODMAP (this bad advice would make me waste 2 months).
She also was quickly to advise alternative medicines. She regularly gave me advice without any argumented explanation.
When her colleague tried to convince me that improving my knees flexibility would allow me to have a better posture, therefore a straighter abdominal cavity, thus letting more space to my intestine, and that should significantly improve my symptoms, I understood that I obviously had to stop relying on the medical community. So I put an end to physiotherapy.
Act 7: I take things charge of the situation
December: I made an update on my illness. I took back my notes, all the interesting articles I found and my diet diary. I wrote nearly everything I ate since the beginning of August and this would prove very useful!
First observation: I was very often sick
Below is a graph of the intensity of my pain grom mid-August to mid-December. The pain index is arbitrary
- 1: My stomach hurts, but I can do pretty much whatever I want.
- 2: It’s better for me to stay home to settle down from time to time, but I can work.
- 3: I’m in enough pain to not be able to work or doing any activity that requires a long-term concentration. I generally have big mood drops and spend most of my time in bed.
- 4 and 5: The pain is severe. I take pain medication, put a kettle, nap….but nothing works. It’s hard to keep my spirit up in these moments.

Second observation: FODMAPs seem to be the key
If the functional colopathy diagnosis was correct, then FODMAPs seemed to be the key. The diet is effective in 86% of the patients cases (source).
I realized that none of the diets recommended by my two gastroenterologists was compatible with a low-FODMAPs diet, contrary to what they told me. I understood that this diet excluded a lot of things and was complicated to implement. I also discovered that the two specialists didn’t know anything about it.
A few days earlier, I had taken back my diet diary and outlined everything that contained gluten (pasta, bread, cakes…) and it was correlated to some episodes, but wasn’t a perfect match, there was inconsistencies. It could as well have been completely random.
Then I found an article explaining that fructans are often confused with gluten in the case of intolerances. Fructans are listed in FODMAPs and are most likely the cause of colopathy symptoms.
I took back my list and the correlation was better. Every time I had eaten a large quantity of fructans, I had been sick. I have a first lead!
I also noticed that I was only sick 6 to 12 hours after ingestion (which is the time it takes for foods to go toward the large intestine, if I understood well).
Second lead, I had an episode almost every time I ate hummus or lentils. My highest pain peaks were precisely due to some homemade coral lentils dhal I prepared without changing the cooking water. Lentils and hummus are rich in GOS.
Third observation: I need help with this diet
I had trouble finding reliable information on FODMAP because there were regularly some contradictory lists.
I tried to remove fructans and GOD from my diet, and it was better! I had fewer episodes and they were less intense, but I was far from solving the problem.
I had a lot questions:
- How could I be sure that fructans and GOS were making me sick?
- Why did I keep getting regularly sick even when I stopped eating them?
- Was I intolerant to other FODMAPs? How could I know?
I took an appointment with the dietician the physiotherapist recommended I cancel.
Act 8: The dietician specialized in FODMAPs and functional colopathy
I finally found someone who seemed competent on the subject. What she was telling me corroborated everything I read.
She read my diet diary and noticed some few mistakes.Fructans are omnipresent in food (wheat, onion, garlic, asparagus, artichoke, …). It was complicated to remove them. Her feedback was very useful and enabled me to improve my diet.
She proposed a very classic but methodical way of proceeding:
- Phase I, FODMAPs exclusion: I remove every FODMAP from the diet (it was very strict) and we wait a few weeks to see if there was a significant drop in symptoms
- Phase II, FODMAPs reintroduction: I reintroduce FODMAPs one by one in the diet and see if any symptom appear
- Phase III, Assessment: We update about guilty products and deduce the FODMAPs to exclude from my diet
She invited me to try and take peppermint oil capsules. I wouldn’t notice any effect.
She also avised me to take Glutamine. Again, no positive effect. I even had a doubt it caused transit disorders. A study showed that it seemed to work for some people… but not for me.
Before the holidays season, I started the elimination phase based on the PDF files she had sent me.
My noted helped me because I could see with certainty that some FODMAPs did not make me empirically sick (like lactose for example). SO I didn’t have to eliminate everything. That is a plus because a strict low-FODMAPs diet is very complex to follow over time.
« A very restrictive diet is often difficult to follow. Prospective studies showed that even if 75% of patients joined the diet, only 12.2% followed it continuously. Since compliance is a key element in the potential success of such a diet, the help of a dietician can be very useful. A very strict diet is impossible to follow for more than 3 or 4 weeks. I this strict diet is beneficial, it is important to determine the doses of FODMAPs that patients can tolerate. »
– National French Gastro-Enterology Society, Low FODMAP diet (source)
Even though the episodes were less intense and less frequent, I still got sick. Was I still making mistakes? Was there anything else that made me sick?
Act 9: The right tools
FODMAPs are not indicated on food labels. So, if I wanted to buy a product, I had to check if ingredients contained some FODMAPs and estimate the amounts (which is often impossible because it is not indicated).
I discovered there is only one laboratory in the world, an Australian University, Monash, that publishes FODMAPs amounts in common food. It is a priori the only reliable FODMAPs information source.
I was continuing the elimination of the 2 FODMAPs that made me sick: fructans and GOS.
Until then, I was using PDF of paper FODMAPs lists. But it became quickly painful to shop with. I often struggled to find an item on the lists and many were missing. I didn’t know their reliability or accuracy. I needed to find better tools to make less mistakes and make my daily life easier.
The FODMAP bot
The first one I found was the FODMAP bot on Facebook. It’s a french bot based mainly on information extracted directly from Monash publications.
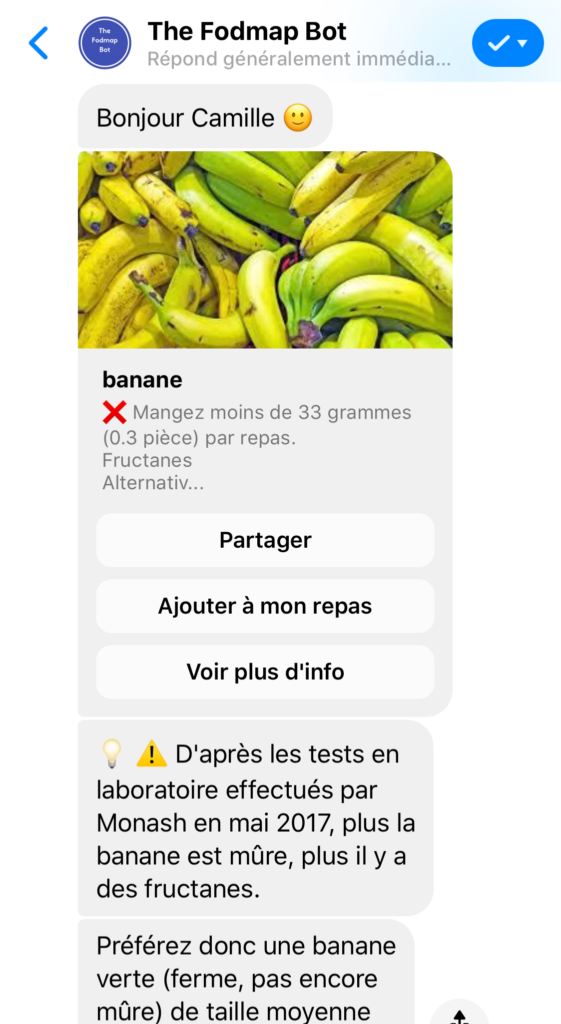
You just have to type the name of the food and it extracts its data. You can even look for several products at the same time. Theoretically, you can also search for complex products (with several ingredients) or even scan the barcode. The app will look for the composition in Open Food Facts.
Bet between OFF’s incomplete information and the lack of FODMAP’s amount data, the information is quickly incomplete and therefore useless for many products. So I stick to looking up simple foods and it already came in very handy.
Another shortcoming is that you can’t specify which FODMAPs you need to avoid from the list. For example, cauliflower (which is rich in mannitol) does not make me sick and I would like the bot to say it’s ok for me.
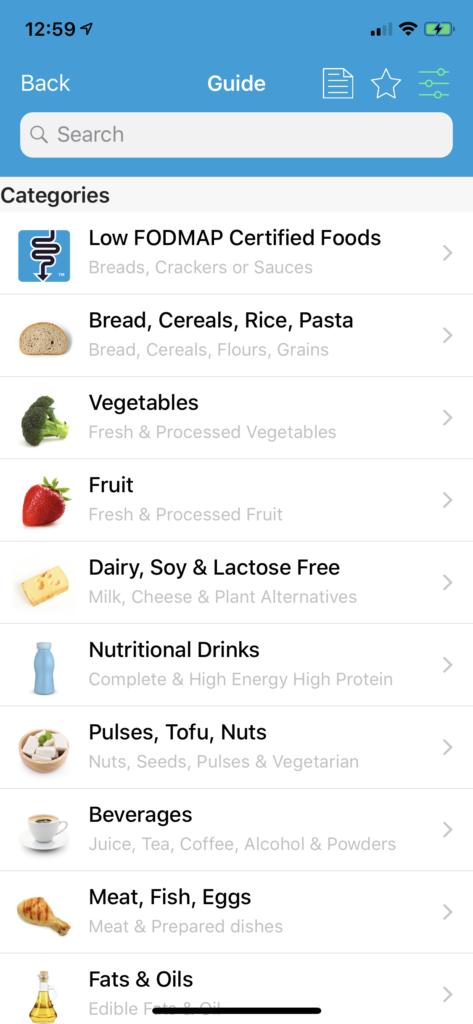
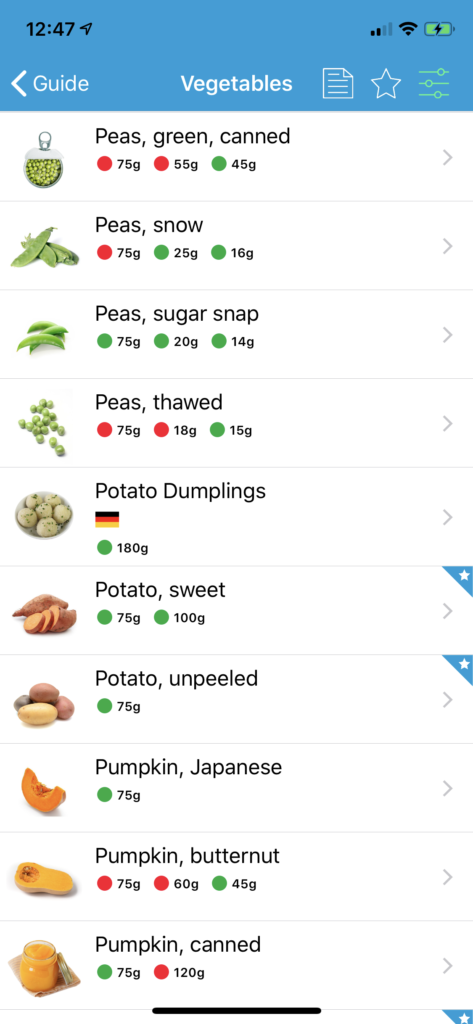
Monash University FODMAP diet app
Monash University is the only reasearch center that publishes measurements of FODMAPs amounts in foods. And they’ve made a whole business out of it!

Their mobile application (available on iOS and Android) gives information directly from the source and is often updated.
It also allows you to define your profile. You can describe your sensitivity to each FODMAP. Therefore when you search for food or browse throught lists, products are color-coded (green, orange or red) depending on your sensitivity.
It has become my default app. The lists are useful for finding new food ideas to buy when I’m shopping.
When I don’t know the name of a product in English, I use to FODMAP bot.
Open Food Facts
Open Food Facts is a French open food products database, powered by everyone.
Its phone app allows you to scan a barcode and get the list of ingredients and nutritional information.
Unfortunately, Open Food Facts do not handle FODMAPs yet.In the meantine, I use the app to easily find the ingredients of the food I eat. This allowed me to just write the name of the product in my diet diary and if I needed to find the list of ingredients, I went back to the app.
Overall, even though they were far from perfect, these tools made my life easier. Finding a recipe, doing my groceries shopping… are far less painful to do now.
Act 10: In search of the last intolerance
During the Christmas holidays, I followed as strictest diet possible in order to take minimal risks. I really ate very few different food. I didn’t try products that I wasn’t sure about. As a result, I managed to spend good holidays with my family which was encouraging.
The only problem was that I only ate rice, spinach, quinoa, French cheese…it became tiring and limiting, especially when I wanted to go out.
I still had confidence in the low-FODMAP diet and continued to follow it strictly.
In February, I finished my tests. I found out that only fructans and GOS make me sick. Mannitol, lactose, fructose and sorbitol do nothing to me, even in large amounts. Unfortunately, I still had regular episodes.
I did blood tests again but everything was OK. I also did a respiratory test at Montpellier Hospital in order to detect lactose intolerance. The first gastroenterologist prescribed it but I couldn’t have an appointment in less than 6 months.
The test is simple: you drink 25g of lactose and every 30 minutes during half a day, they measure the amount of exhaled hydrogen.
If I had known that, I would have drunk 2-3 glasses of milk at home to check. Anyway, I suspected that I had not lactose intolerance and the test confirmed it.
I contacted my dietician again to review my new episodes. As usual, I showed her my dietary diet so that she was able to analyze my latests episodes.
She deduced 2 leads:
- Some ingredients found in processed food known not to be well tolerated
- Histamine
She gave me a list of products that could be the source of my latest troubles
- Guar gum
- Carob seeds flour
- Inulin
- Chicory
- FOS
Act 11: Testing the histamine-free diet
Her main focus was on histamine. When she looked at my latest episodes, she regularly noticed products containing it (dark chocolate, some French cheese,…). It seemed to be an interesting lead to follow.
When I received her document on the low-amines (including histamine) diet, I teared up. The diet was very complex and I still had to exclude fructans and GOS. What I could eat with both of these two diets was really reduced to a small foods list. Most of the foods I bought the day before were excluded by the histamine-free diet. Moreover, histamine (like FODMAPs) is not listed on labels and changes over time.
I’m usually very calm tempered, but my first impulse was to go running to release the pressure because I felt that it was going to be a nightmare!
A few days later, I called my sister so that we could think together about what I would be able to eat. She took the list from the histamine-free diet, I took my low-FODMAP app and we looked for recipe ideas. We ended up having a nervous laughter because it was so hard to find.
At the end of March, I started the histamine-free diet. I started with 4-5 simple recipes. I followed the diet for 15 days. I didn’t notice any change. I reintroduced high-histamine foods step by step and then again, no change.
You’re going to see in the next Act that, in fact, it was easy to deduce that I was not histamine intolerant.
At this stage, I was worried and lost. The diet test had been painful. I was still regularly sick. I asked myself a lot a questions: How many possible intolerance are there? Will the next diets to try be as complex?
The most haunting question was: « Have I done everything there is to do with diets? Maybe the episodes I experience are not directly linked to what I eat and there is nothing to do. »
Act 12: I finally find a diet that works… with some lines of code.
Since the beginning of July 2018, I wrote down almost everything I ate. I also kept a record of every episode, the symptoms, medical appointments… I got around 200 days of data and 70 referenced episodes.
At the beginning, it was just to show what I ate to the first doctor I consulted. Then, I kept the habit for the next doctors, the specialists, the dietician, or just to look for interesting leads by myself.
Mid-April, I woke up with an idea: take all my notes, look for each product if it appears before an episode (4 to 24 hours before) and do statistics. I wanted to find correlations between my foods and my episodes.
My notes were never designed to be interpreted by code. Sometimes I wrote the date in letters, sometimes in numbers, sometimes I started a new day with a dash, sometimes I forgot…
I called Matthieu (my friend and associate at Human Coders) and asked him if he could help me. We spent two days reformating my diary and coding a program that could interpret my lists and put it all into a spreadsheet.
After these two days, I had a list of what I ate with two kinds of information: how many times I ate the food, and how many times I had an episode after I ate it.
The data was far from perfect because I didn’t always use the same name for a food, I sometimes used generic names for different products, I forgot some foods… but with the amount of data I had, I could retrieve some crucial information!
For those who are interested, since then I found apps like The FODMAP Bot or CARA that apparently allow that kind of correlation without a line of code.
The empirical diet
The first thing I did was to display the list of foods that made me the least sick (I considered any foods I ate more than 10 times and with a suspicion rate of less than 25% were safe).

This was a revolution for me! I had in front of me a diet that didn’t make me sick, in a safe way since given it was empirically based on a fairly representative data. This was one of the most decisive steps in my search for a solution. I just wish I had that idea earlier!
For example, I could notice that dark chocolate or cheddar didn’t make me sick at all even though they were very rich in histamine. If I had this spreadsheet earlier, I could have avoided the painful 2 weeks of low-amine diet.
The suspicious products
If I sorted out the spreadsheet the other way around, I got a list of the most suspicious products. But that was not so simple. I didn’t find any suspicious foods that I ate many times. Indeed, generally as soon as I had a doubt on a product 2 or 3 times, I removed it from my diet.
I also had many false positives. I saw several « safe » foods appear because, each time, I ate them before an episode. But it was random.
So, I had little data on suspicious foods.
However, I noticed some foods in that list that did not contain FODMAP, but that I still needed to avoid because they obviously made me sick.
In this list, suspicious products were vanilla ice cream, Monoprix mayonnaise (but not the other brands), Bjorg rice cream, cabbage salad sauce from the sushi restaurant down the street…
After some research, I found the common point: guar gum (E412) and/or carob seed flour (E410). Foods that my dietician had told me about (see Act 10).
If I took into account fructans, GOS, guar gum and carob seed flour, I could explain almost all of the episodes I wrote down in my diary!
Act 13: At least, i find my own diet
At the end of April, I removed guar gum and carob seed flour. It was then again a good challenge because they are very common in processed foods. I found them in some gluten-free breads and biscuits (which I used to buy to avoid wheat which contains fructans), in some mayonnaise and sauces, some ice creams, most of vegetable creams, many pre-prepared meals…
In the span of a few days, my symptoms mostly disappeared. In the following weeks I still had some (small) episodes but every time they were due to a mistake on my part (I ate too much of one of the 4 elements I needed to avoid).
At the time I wrote this article, I had been following this diet for almost 2 months and I’m pleased to announce I’m fine!
I’m gradually finding my own marks when shopping. I usually eat some very basic meals in the few restaurants I know.
I stopped writing daily on my diet diary, writing only my episodes and the 2-3 meals I ate before. In general, I can easily identify the products responsible.
I’m still pretty paranoid about what I eat. I’m progressively introducing new foods, new meals to better know my limits and diversify my diet. With time, I’m becoming more confident in my diet and my health. I started planning things again, making projects, getting back in touch with people I hadn’t seen in a year, inviting people to my house…
Morally, I’m much better. Getting my normal life back helps a lot.
This experience has been long and painful, althought the solution was finally simple and scientifically known for more that 10 years.
What do I eat?
I try to go back to a diet closer to what I used to eat. I eat 100% vegetarian at home again. I suppressed almost all pre-prepared meals, sauces…because they often contain a problematic ingredient and it’s tricky to assess quantities.
For basic products, I tried to find substitution products or tricks. I give you a few examples by categories:
Fructans
Examples of fructanes:
Bread (because of wheat): I replace by gluten-free bread (brand Schär for guar gum-free). I tolerate 2 to 3 slices of white bread, especially if it’s sourdough bread.
Pasta (because of wheat): I switch to gluten-free
Wheat flour: I use flours made of rice, corn, buckwheat…
Artichoke: I buy artichoke hearts in cans.
The list goes on. It’s probably the most constraining category for me.
I suppress many products completely (or I eat them in very limited quantities, strictly following the recommended quantity): asparagus, garlic, onion, beet, leek, peas, dried fruits, bilberry, cashew nuts, some teas and infusions…
Galacto-oligosaccharides (GOS)
Examples of GOS:
Lentils and chickpeas: I eat them in small quantities, in cans, properly washed or cooked by changing the water multiple times
Soy milk: I replace it with other vegetal milks (rice, almond, …)
I don’t buy hummus, falafels or any preparation made of lentils or chickpeas if I don’t know how they were cooked. I also stopped pistachio nuts, cashew nuts, beans…
In sum, I now have my habits and my empirical diet. When I want to eat a new product, I check if it’s safe in the Monash app or if there’s a trick to prepare it (infuse it in oil, buy it in cans, change the cooking water,…)
Guar gum and carob seed flour
Examples of guar gum and carob seed flour:
Ice cream: I now buy Häagen-Dazs or Magnum brands
Gluten-free bread: Most of gluten-free bread found in retail contain guar gum. Some Schär products do not.
Mayonnaise (brand Monoprix): I used to buy the only one on the shelves that contained it! So now I buy any other one and it’s ok.
As it only concerns industrial meals, the simplest solution I found is to scan the barcode with the Open Food Facts app. As these gellant have multiple names, the app is useful to know rapidly if they are contained in a product.
In general, when a product contain some, I check other brands (of better quality) and I usually end up finding one that doesn’t contain any.
How do I eat at the restaurant?
I do not say it’s simple. Since the list of foods I should avoid is long and most restaurant owners have no idea what FODMAPs are, I usually focus on very simple meals.
The dished I eat most often are: Breton pancakes, sushi, fish and chips, steak and mashed potatoes…
I avoid sauces because it is often difficult to know their exact composition.
The dietican advised me to ask if the meals are gluten, garlic and onion-free, and to ask for the sauce on the side. That avoids a lot of surprises, other products are normally indicated or can be sorted out on the plate.
I try to order the same meals, in the same restaurants to limit risks.
How do I eat at my friends’ house?
If they are not already aware of my intolerances, I inform them. It’s very complicated to follow this diet when you’re not familiar with it. As far as possible, I suggest to have a drink instead, to go to a restaurant I know, to bring my own meal…
I they insist on inviting me, I explain the broad outlines of my diet. We look together for a suitable recipe. We list the ingredients and I tell them not to add anything. Out of caution, I usually check with them before eating: « Did you add garlic? Onion? Wheat?… ».
I have no problem watching other people eat or eating something different. I would rather eat a simple meal than risking having another episode!
Edit: Act 14: Respiratory Test for SIBO diagnosis
While doing my research on IBS, I regularly heard about SIBO (Small Intestinal Bacterial Overgrowth).
The link between SIBO and IBS seemed strong. IBS was cited as a risk factor and a symptom for SIBO. In addition, the Wikipedia page on SIBO indicated:
Some studies reported up to 80% of patients with irritable bowel syndrome (IBS) have SIBO (using the hydrogen breath test). Subsequent studies demonstrated statistically significant reduction in IBS symptoms following therapy for SIBO.
When I read that, I wanted to take the test to find out if I hat it. During the summer, I went to my GP to do some tests. She only knew SIBO by name. I showed her the information I had and she gave me a prescription for a Hydrogen Breath Test.
The test is quite simple. With an empty stomach, you swallow glucose (or lactulose) and then blow into a balloon every 20 minutes to measure the quantity of several gas, especially hydrogen. It’s exactly the same principle as the lastose intolerance test I did in February.
The test « unfortunately » came back negative.
So, I don’t have SIBO. I took an appointment with a gastroenterologist specialized on these subjects at the hospial when I took the test.
Edit: Act 15: The specialized hospital gastroenterologist
Following the respiratory tests, I decided to take an appointment with a specialist to check if there was still tests to do, if I could still make progress in the diagnosis, or if I did everything possible for now.
For that last appointment, I was not in a hurry. I chose the « best of gastroenterology » in Montpellier, advised by my GP and a few people I met during the respiratory tests at the hospiral. I didn’t know if he was good, but he was very busy because I had to wait more than 6 months for an appointment!
In December 2019, I finally went to see him. I was welcomed by 2 internes. I explained my situation to them, gave them my thick medical record.
Contrary to the liberal gastroenterologists I saw before, they proceeded methodically. They questionned me and asked for my documents one by one.
Quickly, their conclusion was clear: I had done every test I could, I had a functional colopathy and I didn’t have SIBO.
Good news: I was done with my medical journey.
Bad news: It confirmed I suffered from a poorly known disease, for which there was not much to do except a strict diet and some medication to manage symptoms.
One of the interns took the occasion to give information about the disease to the other intern, especially about its multi-factor aspect and some means to act on it. She drew a pie chart composed of the following parts:
- Chronic Inflammatory Diseases of the Intestine
- Genetics
- IBS, Microbiota > Prebiotics
- Environment (tobacco, stress…) > hypnosis, antidepressant, smoking cessation
- Diet > low-FODMAPs diet
With me, she quickly focused on prebiotics. She advised me to take Psyllium, (SPAGULAX,. sold in pharmacy) because she thought it was better to start with it.
Strangely, she avoided the point on low-FODMAP diet. I explained that in my case, it was THE only thing that allowed me to feel much better. She explained that they avoid talking about it too much because it regularly leads to malnutrition issues.
I explained to her that in my case, it was the opposite. I lost 5 kg the first months because I preferred to be a little hungry on a regular basis than to take the risk of eating something that could make me sick. (especially between meals). It was only when I managed to follow the low-FODMAP diet correctly that I regained weight, because I was eating when I was hungry again and wasn’t afraid to snack when I was hungry anymore. In my opinion, we needed to talk about this diet. It was one of the few « solutions » that had been scientifically proven. Nevertheless, I thought it had to be accompanied. Giving a small list full of errors wasn’t useful. On the other hand, suggesting updated apps, prescribing appointments to a dietician, explaining the 3 phases of the diet, checking up with the patient over time… I thought it was useful.
Then the professor entered the room. His interns summarized the situation. He came back to the subject of FODMAPS and emphasized the risk of malnutrition. I explained again what I was just saying to the interns.
He offered me a document describing the diet. It was the one he gave all his patients that needed to follow it. I showed him it contained errors.
For example, like the ones I had been handed before, it advised eating bananas, however ripe bananas are rich in fructans. It was short, therefore incomplete. It didn’t say, for example, to avoid dried grapes, which are very rich in fructans. I didn’t allow to follow the diet correctly without being sick.
I ended the appointment by introducing them to the Monash app and the FODMAP bot. The doctor gave me his personal phone number so that I could send him the links when I got out of the hospital. I was great that he was open minded and ready to question himself. On the other hand, I was having a hard time understanding he was so poorly informed on the diet. I hope he’s educated since and will spread the word to his colleagues.
My medical journey is now over. All I have to do now is to go on and learn to live with the disease, hoping my situation will eventually improve.
Conclusion
If 10% of the world’s population suffers from functional colopathy (source) and low-FODMAP diet has a beneficial effect on 86% of patients (source), how do we explain I was so badly accompanied and advised, when IBS represents 10 to 15% of consultation reasons to GPs and more than one third of consultations with the gastroenterologist (source) (and that all the people in my situation that I recelt came across make the same observation).
I emerge from this experience with many questions.Why do some doctors know almost nothing about functional colopathy (sometimes even the name)?Why can’t some gastroenterologists diagnose it and how can they know so little about the low-FODMAP diet?Why do doctors who are unfamiliar with the disease give advice and prescribe treatments?Why is it so difficult to find safe and updated information about this disease on the internet?Why is there so few apps to make our lives easier?
I insist on the fact that I am not a doctorat and that you should question the medical information I wrote in this article.I wrote it to narrate my personal story, not to describe a miracle diet. What worked for me, may not work for you. Note that it’s important to consult a doctor for a reliable diagnosis (and therefore exclude other serious diseases which are important to detect as soon as possible).
I would like to thank Matthieu and Sabine, my associates at Human Coders and MerciCookie respectively, who juggled with my constraints. The freedoms in our way of working that we had given each other, which had been a luxury until now, became a necessity during this period.
Thanks also to the manager of the sushi shop down the street who is going to change the mayonnaise recipe just for me. Thanks also to my dietician who gave me valuable information.
Last but surely not least, I would like to thank my family and friends who accompanied and supported me throughout this period. Thanks to all those who were there whenever I needed them, even when I regularly stood them up, and probably fed them up talking non stop about my disease, …
Finally, good luck to all the sick people who are going through a similar adventure. I hope I have been able to give you some clues, some courage and some motivation.
PS: I’m not a doctor, so I won’t answer any medical questions. On the other hand, if you have any specific question about my case, don’t hesitate to ask in comment, I’m going to answer them with great pleasure. If patient associations, journalists, doctors… wish to contact me, you can send me an e-mail.
Thank you to Guilaine Grémy and Léa Bunnens for their collaboration concerning the translation in English of my article.
You can read the French original version here: https://www.camilleroux.com/2019/06/18/syndrome-de-lintestin-irritable-recit-dun-parcours-medical-seme-dobstacles/

I can only say thank you! I have exactly the same experience and am now trying to find my own diet. I am as baffled as you by the ignorance of the medical profession. In part, I believe they are caught up in the traditional role of the doctor, which is to prescribe medications rather than give good advice. And what would the Pharma industry do if we all cured ourselves?
Hi Camille. I hope this comment finds you well. I am astonished at your story because it sounds exactly like mine. I am getting ready to do a colonoscopy afraid that the laxative medication itself could kill me. but I have been to over 6 gastro’s each more clueless than the last. funny thing is my symptoms started when I moved to France and I have been here for 4 years. and I know most of my friends suffer from gastro issues here. I am sure that no one in France can help me they seem to be stuck in the French mentality in that there is only one way to do things. So this year I am going to pay 1500 euro to an American who does a holisitc approach by testing the stool and doing an in depth analysis of the stool called GI MAP which is a test provided in most countries but not France :) ironic. but she does the test and gives support and advice. which would be the same price as doing colonosccopy fibroscopy once a year